Tear Gas, Pepper Spray, and Rubber Bullets: A Primer
By James Chenoweth MD MAS
Recent protests over the murder of George Floyd by police in Minneapolis, Minnesota have often been met with police use of “non-lethal” (better described less lethal) forms of crowd control/dispersal. The most common of these include tear gas, pepper spray, and impact rounds (beanbag rounds and rubber bullets). Emergency physicians and toxicologists should know what compounds these devices contain and the risks associated with their use by police.
Tear Gas
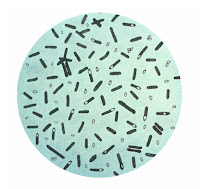
Tear gas is a heterogenous group of compounds that are irritant gases which cause coughing, eye irritation, and skin irritation upon exposure. The most common of these compounds in current us is CS (chlorobenzylidene malononitrile) gas. CS was developed in 1928 and is named after its creators, Corson and Stoughton. It was first used by the British Army in 1958 and was frequently used by the US military during the Vietnam War.1 The military use of chemical weapons, including those used in riot control was banned by the Chemical Weapons Convention which was ratified by the senate in 1997.2 This convention does not ban police use. CS is a solid at room temperature and must be either dissolved in a solvent, micro pulverized into a powder, melted and sprayed in molten form, or heated in thermal grenades and released as a hot gas.
A variety
of CS devices used against protesters in Istanbul, Turkey (picture
source: https://en.wikipedia.org/wiki/CS_gas)
Toxicity
CS gas is a potent irritant of mucous membranes. Upon
contact it causes immediate pain and irritation of the eyes, nose, mouth, and
skin. It acts through activation of transient receptor potential (TRP) channels
on nociceptors (pain receptors, specific target is TRPA1). Activation of these
receptors leads to the immediate sensation of pain and reflex lacrimation.3
Most people exposed to CS gas will experience transient irritation and pain of
the eyes, mouth, nose, and skin. These effects typically subside over 10-30
minutes after removal from the exposure.4
More serious effects have been reported. With significant contact to the eye more serious injuries including corneal stromal edema, conjunctival tearing, glaucoma, and deep vascularization can occur.5 Skin burns may occur due to contact with heated CS from incendiary cannisters and massive chemical exposure.6 Allergic reactions have been reported and there is evidence that CS may be a sensitizing agent.3,7,8 Ingestion of CS gas can cause gastrointestinal irritation, nausea, and vomiting.9 Cardiovascular effects include tachycardia and hypertension may occur, likely secondary to the pain associated with exposure.3
Deaths have been reported after prolonged exposure in enclosed spaces, most often in prisons. Death typically occurs from pulmonary irritation leading to pulmonary edema and respiratory failure. Organic solvents may contribute to this toxicity.3,10,11 Some deaths have also occurred due to direct impact of tear gas cannisters or explosive munitions.3,12 CS has also been associated with an increased risk of spontaneous abortion, which lead Chile to suspend its use in 2011.3
Of particular interest currently, CS exposure has been linked to increased respiratory illness.13 In a prospective observational study of military recruits undergoing mask confidence training (this training involves taking off a gas mask while in a room filled with CS gas), recruits were more likely to develop an acute respiratory infection in the 7 days after CS exposure than the 7 days prior (RR=1.79, 95%CI=1.29, 2.47).14 The current use on large crowds of protesters in the setting of the SARS-CoV-2 pandemic raises questions regarding what increased risk of infection those exposed to CS may experience.
Treatment
The first step in the treatment of CS exposure is to remove the person from exposure. CS is heavier than air so lifting exposed persons off the ground and taking them to a ahigher elevation will decrease additional exposure. Once removed from exposure, soap and water decontamination should be performed to remove any remaining CS from the skin. If burns are present, water or alsine irrigation may be effective and less painful.1 For ocular exposures, contact lenses should be immediately removed followed by copious saline or water irrigation for 10-20 minutes. If irrigation is being performed in a healthcare setting, topical anesthetics may be used to decrease pain and blephorospasm.2 Some have advocated for the use of baby shampoo to aid in decontamination of the face and eyes. While mechanistically this should improve removal of CS that has been dissolved in organic solvents, a randomized trial found no difference in discomfort between a baby shampoo and a water alone group.15
To protect healthcare providers from potential exposure, clothes should be removed (if possible) prior to entering any enclosed space. Patients should be evaluated for possible traumatic injuries or burns due to direct impacts, explosives, and incendiary devices.
Prevention
Healthcare providers caring for participants in protests where CS has or may be used can take measures to protect themselves. Chemistry goggles without ventilation holes can significantly decrease eye exposures. Half or full-face respirators can decrease exposure (check manufacturer filter specifications).16 P100 filters would be preferred as they are protective against petroleum based products.
Pepper Spray (including pepper balls)
Pepper spray is commonly used for crowd control and personal protection. The primary component is oleoresin capsaicin (OC) a purified form of capsaicin which is found in plants from the genus Capsicum. It is typically dissolved in propylene glycol and water then pressurized in a spray cannister. OC was developed in the 1970’s and gained use by police departments in the 1980’s.1 Mace is a brand of protective spray that originally contained chloroacetophenone (CN) which is similar to, but more toxic than CS. CN has mostly been replaced in Mace by OC although a “triple action” formulation still exists that contains CN, OC, and an ultraviolet marker dye.17
Pepper balls are frangible spheres filled with irritant powder or liquid. This powder may be OC or a similar compound called pelargonic acid vanillylamide (capsaicin II), a capsaicinoid derived from chili peppers. Pepper balls are typically fired from specially designed launchers or paintball guns.
Toxicity
OC and other capsaicinoids act on TRP channels, similarly to CS gas (although the specific target is TRPV1 for OC). Activation of these receptors leads to the immediate sensation of pain and reflex lacrimation.3 Similar to CS, most people exposed to OC will experience transient irritation of the eyes, mouth, nose, and skin. These effects typically subside over 1.5 to 2 hours after decontamination.18
Direct ocular toxicity is of primary concern as OC is often intentionally sprayed at a person’s face. Exposure does not typically cause irreversible eye effects. However, more severe ocular injuries have been reported, including hyphema, uveitis, necrotising keratitis, coagulative necrosis, symblepharon, secondary glaucoma, cataracts and traumatic optic neuropathy and loss of sight.2 Solvents used as carriers for OC may also contribute to corneal injury.19 There is also evidence that corneal sensation can also be affected, leading to decreased blink reflex. This effect can last up to 7 days.18
Dermal effects are typically mild and consist of burning sensation and pain. In a small number of patients (2.8% in one study20) more severe dermatologic injuries may occur. These include burns, contact dermatitis, and blister formation.21 Exposure to mucous membranes causes severe irritation. This can manifest and rhinorrhea, cough, sore throat, and hoarse voice.21,22 Respiratory symptoms are reported but typically mild. In a study of healthy volunteers, inhalation of OC was not associated with any decrease in FEV1.23 In a retrospective review 2 of 12 (16.7%) patients with asthma presented with respiratory symptoms compared to 3 of 82 (3.7%) without prior asthma diagnosis.24
In rare cases more severe toxicity may occur. Laryngeal edema and chemical pneumonitis have been reported follow inhalational exposure.21 There are many reports of deaths following OC exposure. Between 1993 and 2015, over 70 in custody deaths have occurred after OC exposure.21 Amnesty International estimates that more than 100 in custody deaths have occurred following OC exposure since 1990.25
Direct impact injuries leading to permanent vision loss have been reported, particularly with pepper balls. At least one death has been connected to traumatic injuries suffered following pepper ball use by police.26
Treatment
Treatment of OC exposures are very similar to those used for CS exposure. The first step in treatment of OC exposure is to remove the person from the exposure. Once removed from exposure, soap and water decontamination should be performed to remove any remaining OC from the skin. Skin should be blotted dry to avoid spreading any residual OC residue.21 If burns are present, water or saline irrigation may be effective and less painful.1 For ocular exposures, contact lenses should be immediately removed followed by copious saline or water irrigation for 10-20 minutes. If irrigation is being performed in a healthcare setting, topical anesthetics may be used.2 Washing with a mild, oil-free soap will help break down the OC resin and speed up its removal.19
Several agents have been reported to decrease the burning pain associated with dermal exposure to OC. Magnesium-Aluminum hydroxide has been reported to decrease the burning pain following capsaicin exposure.27 Vegetable oil or vinegar also may be more effective than water alone for decreasing pain after dermal exposure.21,28 However, a randomized trial of several methods of decontamination (aluminium hydroxide– magnesium hydroxide, 2% lidocaine gel, baby shampoo, milk, or water) found no significant difference between these decontamination methods.29 Of the potential decontamination methods, only baby shampoo and water/saline would be considered safe for ocular exposures. Patients should also be counseled on the risk of decreased corneal sensation and provided with eye lubricants prior to discharge. Taping the eyes shut while sleeping may also be useful to decrease risk of corneal injury.
To protect healthcare providers from potential exposure, clothes should be removed (if possible) prior to entering any enclosed space. This is particularly true if pepper balls were used, as these may contain a powder than can re-suspend in air with movement of clothing. Patients should be evaluated for possible traumatic injuries or burns due to direct impacts. This is of particular concern for direct ocular impact from pepper balls.
Prevention
Healthcare providers caring for participants in protests where OC or pepper balls have or may be used can take measures to protect themselves. Chemistry goggles without ventilation holes can significantly decrease eye exposures. These can also protect the eyes against direct impact from pepper balls. Half or full-face respirators can decrease exposure (check manufacturer filter specifications).16 P100 filters would be preferred as they are protective against petroleum based products.
Rubber Bullets/Bean Bag rounds
While not toxicology related, no discussion of less lethal methods of crowd control is complete without mention of impact projectiles, commonly called rubber/plastic bullets and bean bag rounds. Rubber/plastic bullets (also known as baton rounds) were developed by the British Ministry of Defense for use in Northern Ireland in 1970.30 They are a heterogenous group of projectiles typically made of elastic material, such as rubber, which may surround a central metallic core. Newer foam capped plastic projectiles are also included in the category of rubber bullets.30,31 They are powered by a low power propelling charge and have a reported muzzle velocity of 200-220 feet per second (~136-150 mph).30 These projectiles were originally intended to be fired into the ground and bounce into the lower extremities. They are not supposed to be fired directly at a person except in cases of imminent danger.30
A selection of baton
rounds (rubber bullets) (picture source: http://quarryhs.co.uk/baton.htm)
Bean bag rounds are a form of impact round that consists of
a small fabric “pillow” filled with lead shot. This is fired from a modified
shotgun and has a muzzle velocity of 230-300 feet per second (156-204 mph).32
Example
bean bag rounds (Picture source: https://www.reliasmedia.com/articles/131518-less-lethal-force)
Early in their use, the risks associated with rubber bullets were well known. A case series of 90 patients in 1975 showed 1 death, 41 patients requiring admission to the hospital, and 17 patients with permanent disability. The authors found that direct impacts to the face and neck were associated with the worst injuries.33 Despite this, these devices continue to be used for crowd control, often resulting in serious injury. A systematic review by Haar et. al34 in 2017 found 1,984 patients with injuries from kinetic impact rounds reported in the medical literature between 1990 and 2017. In their review there were 53 deaths and 300 people who suffered permanent disability. These most frequently resulted from strikes to the head and neck (49.1% of deaths and 82.6% of permanent disability).34 Serious injuries, defined as injuries requiring professional medical management, occurred in 71% of cases.34
The authors of this review cite their findings in a call to decrease to use of these rounds for crowd control. They note that these rounds are known to be inaccurate and that police often aim them at the head and neck, increasing the risk for permanent disability or death. During the current protests, there are multiple media reports of serious injuries cause by these rounds, including a reporter who suffered permanent eye damage.
Conclusion
It is clear that techniques often described as non-lethal can result in serious injury and death. Healthcare professionals and media organizations should stop describing them as such. The use of CS, OC, and impact rounds for crowd control should be also re-examined, and police should be better trained to avoid aiming impact rounds and pepper balls at the head and neck. The use of these methods on peaceful crowds should be condemned. Healthcare professionals should be aware of the risks associated with the use CS, OC, and impact rounds as well as how to care for patients injured during protests.
References
1. Tidwell
RD, Wills BK. Tear Gas (Pepper Spray) Toxicity. In: StatPearls. Treasure Island (FL)2020.
2. Schep LJ, Slaughter RJ, McBride DI.
Riot control agents: the tear gases CN, CS and OC-a medical review. J R Army Med Corps. 2015;161(2):94-99.
3. Rothenberg C, Achanta S, Svendsen
ER, Jordt SE. Tear gas: an epidemiological and mechanistic reassessment. Ann N Y Acad Sci. 2016;1378(1):96-107.4. Olajos EJ, Salem H. Riot control agents: pharmacology, toxicology, biochemistry and chemistry. J Appl Toxicol. 2001;21(5):355-391.
5. Gray PJ, Murray V. Treating CS gas injuries to the eye. Exposure at close range is particularly dangerous. BMJ. 1995;311(7009):871.
6. Zekri AM, King WW, Yeung R, Taylor WR. Acute mass burns caused by o-chlorobenzylidene malononitrile (CS) tear gas. Burns. 1995;21(8):586-589.
7. Shmunes E, Taylor JS. Industrial contact dermatitis. Effect of the riot control agent ortho-chlorobenzylidene malononitrile. Arch Dermatol. 1973;107(2):212-216.
8. Varma S, Holt PJ. Severe cutaneous reaction to CS gas. Clin Exp Dermatol. 2001;26(3):248-250.
9. Anderson PJ, Lau GS, Taylor WR, Critchley JA. Acute effects of the potent lacrimator o-chlorobenzylidene malononitrile (CS) tear gas. Hum Exp Toxicol. 1996;15(6):461-465.
10. Chapman AJ, White C. Death resulting from lacrimatory agents. J Forensic Sci. 1978;23(3):527-530.
11. Hu H, Fine J, Epstein P, Kelsey K, Reynolds P, Walker B. Tear gas--harassing agent or toxic chemical weapon? JAMA. 1989;262(5):660-663.
12. Clarot F, Vaz E, Papin F, Clin B, Vicomte C, Proust B. Lethal head injury due to tear-gas cartridge gunshots. Forensic Sci Int. 2003;137(1):45-51.
13. Hout JJ, White DW, Artino AR, Knapik JJ. O-chlorobenzylidene malononitrile (CS riot control agent) associated acute respiratory illnesses in a U.S. Army Basic Combat Training cohort. Mil Med. 2014;179(7):793-798.
14. Hout JJ WD, Stevens M, Stubner A, Arino A, and Knapik J. Evaluation of an Intervention to Reduce Tear Gas Exposures and Associated Acute Respiratory Illnesses in a US Army Basic COmbat Training Cohort. The Open Epidemiology Journal. 2014;7:37-45.
15. Stopyra JP, Winslow JE, 3rd, Johnson JC, 3rd, Hill KD, Bozeman WP. Baby Shampoo to Relieve the Discomfort of Tear Gas and Pepper Spray Exposure: A Randomized Controlled Trial. West J Emerg Med. 2018;19(2):294-300.
16. NIOSH. alpha-Chloroacetophenone. 2019; https://www.cdc.gov/niosh/npg/npgd0119.html. Accessed June 1, 2020.
17. Leu C. What's Inside Triple-Action Mace? Chili Peppers and UV Dye. 2017; https://www.wired.com/story/whats-inside-triple-action-mace-chili-peppers-and-uv-dye/. Accessed June 1, 2020.
18. Zollman TM, Bragg RM, Harrison DA. Clinical effects of oleoresin capsicum (pepper spray) on the human cornea and conjunctiva. Ophthalmology. 2000;107(12):2186-2189.
19. Lee RJ, Yolton RL, Yolton DP, Schnider C, Janin ML. Personal defense sprays: effects and management of exposure. J Am Optom Assoc. 1996;67(9):548-560.
20. Kearney T, Hiatt P, Birdsall E, Smollin C. Pepper spray injury severity: ten-year case experience of a poison control system. Prehosp Emerg Care. 2014;18(3):381-386.
21. Yeung MF, Tang WY. Clinicopathological effects of pepper (oleoresin capsicum) spray. Hong Kong Med J. 2015;21(6):542-552.
22. Geppetti P, Fusco BM, Marabini S, Maggi CA, Fanciullacci M, Sicuteri F. Secretion, pain and sneezing induced by the application of capsaicin to the nasal mucosa in man. Br J Pharmacol. 1988;93(3):509-514.
23. Chan TC, Vilke GM, Clausen J, et al. The effect of oleoresin capsicum "pepper" spray inhalation on respiratory function. J Forensic Sci. 2002;47(2):299-304.
24. Watson WA, Stremel KR, Westdorp EJ. Oleoresin capsicum (Cap-Stun) toxicity from aerosol exposure. Ann Pharmacother. 1996;30(7-8):733-735.
25. USA: Excessive and lethal force? Amnesty International’s concerns about deaths and ill-treatment involving police use of Tasers. https://www.amnestyusa.org/reports/usa-excessive-and-lethal-force-amnesty-internationals-concerns-about-deaths-and-ill-treatment-involving-police-use-of-tasers/. Accessed June 1, 2020.
26. Stern DK DR, Gittens RP, How JW, James SI, King PJ, and Stone CE. Commision Investigating the Death of Victoria Snelgrove. 2005; https://web.archive.org/web/20110610210149/http://www.cityofboston.gov/police/pdfs/report.pdf. Accessed June 1, 2020.
27. Lee DC, Ryan JR. Magnesium-aluminum hydroxide suspension for the treatment of dermal capsaicin exposures. Acad Emerg Med. 2003;10(6):688-690.
28. Jones LA, Tandberg D, Troutman WG. Household treatment for "chile burns" of the hands. J Toxicol Clin Toxicol. 1987;25(6):483-491.
29. Barry JD, Hennessy R, McManus JG, Jr. A randomized controlled trial comparing treatment regimens for acute pain for topical oleoresin capsaicin (pepper spray) exposure in adult volunteers. Prehosp Emerg Care. 2008;12(4):432-437.
30. Metress EK, Metress SP. The anatomy of plastic bullet damage and crowd control. Int J Health Serv. 1987;17(2):333-342.
31. Kobayashi M, Mellen PF. Rubber bullet injury: case report with autopsy observation and literature review. Am J Forensic Med Pathol. 2009;30(3):262-267.
32. Ijames S. In defense of the 12-gauge "bean bag" round. 2005; https://web.archive.org/web/20080905235252/http://www.policeone.com/writers/columnists/SteveIjames/articles/118328. Accessed June 1, 2020.
33. Millar R, Rutherford WH, Johnson S, Malhotra VJ. Injuries caused by rubber bullets: a report on 90 patients. Br J Surg. 1975;62(6):480-486.
34. Haar RJ, Iacopino V, Ranadive N, Dandu M, Weiser SD. Death, injury and disability from kinetic impact projectiles in crowd-control settings: a systematic review. BMJ Open. 2017;7(12):e018154.




Comments
Post a Comment