There's Botulism in the Cheese
All suspected cases of botulism should be reported to the CDC and your local health department
A recent outbreak of botulism in Northern California has been linked to gas station nacho cheese. At the time of writing this, at least 9 people have been hospitalized for this rare disease and one has died. But what is botulism?
The History
The first reported cases of food-borne botulism were described between 1817 and 1822 by Justinus Kerner. Dr. Kerner described, in detail, a syndrome of descending paralysis that was linked to eating contaminated blood sausage. It is from this link that we got the name botulism, which comes from the Latin word for sausage botulus. The bacterium responsible for botulism, Clostridium botulinum, was first discovered in 1895 by the microbiologist Emile Pierre van Ermengem after an outbreak linked to inadequately cured ham. The toxin was first isolated in 1928 and the toxin's ability to block neuromuscular transmission was discovered in 1949.
The medicinal use of botulinum toxin type A (Botox©) was first used medically in 1980 for strabismus (crossed eyes) and blepharospasm (excess blinking). It was approved by the FDA for these purposes in 1989. It was not until 2002 that botulinum toxin type A gained FDA approval for treatment of glabellar lines (wrinkles), the use most commonly associated with the brand. Botulinum toxin type A now has FDA indication for a wide variety of cosmetic, glandular, and musculoskeletal disorders.
The Bacteria
The Toxin
A total of 7 strains of botulinum toxin have been identified. They are named toxins A-G and affect a variety of species. Toxins A, B, and E-G cause disease in humans. Toxins C and D affect mammals and birds and type E causes botulism in fish. Botulinum toxin is one of the most potent toxins known, with a median lethal dose of 1ng/kg. To put that in perspective, 1 gram of purified botulinum toxin has the potential to kill 1 million people if left untreated. It for this reason that botulinum toxin is classified as a Bioterrorism Category A (highest potency and potential risk) substance alongside anthrax, plague, smallpox, tularemia, and viral hemorrhagic fevers (such as Ebola).
Botulinum toxin works primarily at the neuromuscular junction. The neuromuscular junction is the site where nerve transmission is converted to muscle contraction. This process involves the release of the neurotransmitter acetylcholine into the space between the nerve and muscle cell. Acetylcholine is stored at the end of the nerve in vesicles. These vesicles must fuse with the cell wall in order the release acetylcholine. This fusion is dependent on a complex of proteins called SNAP and SNARE proteins. Botulism toxin cleaves these proteins and prevents fusion of the vesicle and thus acetylcholine release. The exact site on each protein depends on the strain of toxin but the end result is the same for all forms of botulism: loss of the ability to use acetylcholine to cause muscle contraction. The sites that depend on this include all voluntary muscles including the facial muscles that allow you to smile, the muscles that coordinate swallowing, the muscles in your arms and legs, and those responsible for breathing.
Botulism Syndromes
There are 6 commonly recognized botulism syndromes that vary based on the source of toxin exposure (pre-formed toxin vs bacterial infection/colonization). These syndromes are: wound botulism, infant botulism, food-borne botulism, adult intestinal toxemia botulism, iatrogenic botulism, and inhalational botulism.
Wound botulism (15% of cases)
Wound botulism is caused by an infection of C. botulinum in the skin. It is classically associated with subcutaneous injection ("skin popping") of black tar heroin. Injection under the skin can lead to infection and abscess formation which provides the ideal environment for spore germination and toxin production. This form of botulism is most common in long term heroin users, particularly on the west coast where black tar heroin is more common.
Infant botulism (63% of cases)
Infant botulism occurs when infants <1 year old ingest C. Botulinum resulting in gut colonization due to the lack of normal gut bacteria that would prevent C. botulinum from becoming established. The bacteria in the gut then produces botulinum toxin which is absorbed in the GI tract. Infant botulism is classically associated with ingestion of honey, although this link is only present in ~20% of cases. Infant botulism is the most common form of botulism and results in ~100 cases a year in the United States.
Food-borne botulism (18% of cases)
Food-borne botulism, the form linked to the cases in Northern California, is caused by the ingestion of pre-formed toxin. This is most commonly associated with home canned foods (particularly vegetables with low acid content such as peppers, beans, mushrooms, and beats) or low acid foods that are allowed to ferment at room temperature. Approximately 39% of food-borne botulism cases in the US occur in Alaska where traditional foods such as fermented fish and fish eggs are common. Soft cheeses are also susceptible if they are improperly refrigerated, which is the suspected cause of the Northern California cases.
Adult intestinal toxemia botulism (rare)
Adult intestinal toxemia botulism is a rare form a botulism that occurs in adults and results from intestinal colonization by C. Botulinum. This occurs in persons with abnormal gut anatomy or function, or in those on antibiotics that interfere with normal gut bacteria.
Iatrogenic botulism (rare)
Iatrogenic (caused by medical exam or treatment) botulism occurs when commercially available botulinum toxin products are improperly injected. If the toxin is injected in excessive doses or in improper locations, systemic absorption of toxin may occur. This type of error most commonly occurs when injections are performed by untrained or unlicensed practitioners.
Inhalational botulism (rare)
Inhalational botulism occurs when spores are inhaled from the environment. This was previously reported in 1962 in 3 veterinary workers who inhaled toxin from animals they were caring for. Given the rarity of this type of exposure, inhalational botulism cases would be presumed to be due to bioterrorism unless a definite alternate source could be identified.
Patient Symptoms
The symptoms of botulism can be very difficulty to initially identify. GI symptoms can be confused with other forms of food poisoning and neurologic symptoms can initially be vague. This combined with the rarity of the disease makes early diagnosis of botulism difficult.
Initial symptoms
A preceding syndrome of nausea, vomiting, and abdominal pain may occur with food-borne botulism and is virtually indistinguishable from other forms of food poisoning. Wound botulism patients may have a preceding fever and may notice skin signs of cellulitis (skin infection) or abscess formation.
Incubation period
The incubation time period for progression to neurologic symptoms varies by syndrome. Food-borne, inhalation, and iatrogenic botulism have a typical incubation period of 12 hours to 10 days with most cases developing symptoms within 24-36 hours. Wound botulism has a longer incubation period of 1-2 weeks but may be longer. Infantile botulism typically occurs 3-30 days after exposure. Adult intestinal toxemia botulism is a relapsing syndrome which makes the precise incubation period difficult to identify.
Neurologic Symptoms
Botulism is characterized by a descending muscle weakness. This weakness begins in the face with the muscles around the eyes which can result in double vision. Pupils may become dilated resulting in blurred vision. Often the first symptoms that a patient will present with are facial weakness or difficulty swallowing. This weakness progresses to a descending flaccid (floppy, no tone) paralysis of the upper and then lower extremities. The most feared and life threatening complication is paralysis of the diaphragm and intercostal (between the ribs) muscles which can result in respiratory failure (inability to breath). Without treatment or supportive care, botulism carries a mortality rate of ~50%.
Diagnosis
Initial diagnosis of botulism is based on clinical symptoms and history. A combination of nerve conduction and motor testing may be helpful in differentiating from alternate causes of weakness. However these tests cannot distinguish between botulism and other causes of weakness that target the neuromuscular junction (ie myasthenia gravis, Lambert-Eaton syndrome, or the intermediate syndrome of organophosphate pesticide poisoning). Laboratory testing can be done to identify C. botulinum in the stool or botulinum toxin in the blood, stool, or food.
The standard test performed to confirm botulism is the mouse lethality assay. In this study, a sample (either serum, stool, or food sample) is injected into the abdomen of a mouse. A sample along with antitoxin is injected into a control mouse and they are observed for symptom development. This test can detect very small amounts of toxin but may take several days to complete which limits the test's utility for early diagnosis. The mouse lethality assay is more commonly used as a confirmatory test, particularly in patients receiving antitoxin therapy. Samples must be sent prior to the administration of antitoxin.
Treatment
Supportive care is the mainstay of treatment for botulism cases. Death most commonly occurs due to weakness of the muscles responsible for breathing. The strength of these muscles can be evaluated by measuring the negative inspiratory force (NIF) that a patient can produce. This test essentially measures the amount of suction a patient produces when they breath in. A force of less than -30 cm H20 represents severe respiratory muscle weakness. In such cases, a breathing tube and ventilator are often required.
In cases of wound botulism, wound debridement should be performed as soon as possible. Antibiotic therapy with penicillin will kill C. botulinum bacterial but will not prevent absorption of pre-formed toxin. Antibiotics such as clindamycin and aminoglycosides (such as streptomycin, gentamycin, neomycin, and amikacin) should be avoided as they can interfere with neuromuscular transmission.
Antitoxin
Early administration of antitoxin is critical for stopping the progression of botulism symptoms. The antitoxin binds botulinum toxin in the blood and prevents it from interfering further with the neuromuscular junction. Early treatment with antitoxin is associated with shorter duration of symptoms and decreased ventilator need. A specific form of antitoxin derived form the plasma of immunized humans is available for treatment of infant botulism. It is important to note that antitoxin only halts the progression of symptoms and will not reverse any weakness that is already present. Antitoxin is obtained from the CDC through the local health department.
Prognosis
Botulism has a highly variable duration of symptoms, in many cases lasting more than a year. Following recovery, patients with often report ongoing fatigue, dry mouth, muscles weakness, and decreased exercise tolerance. Despite these symptoms full recovery is possible with proper medical care.
DISCLAIMER
The information in this blog is for information purposes only and is not intended for use in diagnosing a disease or to provide specific treatment recommendations. For information on management of poisoned patients or if you are concerned that you have been poisoned, please contact your local poison center at 1-800-222-1222.
References
[3] Sobel J. Botulism. Clin Infect Dis. 2005;41:1167-73.
[4] Wikipedia. Botulism. Available at: https://en.wikipedia.org/wiki/Botulism. Accessed 5/25/2017.
A recent outbreak of botulism in Northern California has been linked to gas station nacho cheese. At the time of writing this, at least 9 people have been hospitalized for this rare disease and one has died. But what is botulism?
The History
The first reported cases of food-borne botulism were described between 1817 and 1822 by Justinus Kerner. Dr. Kerner described, in detail, a syndrome of descending paralysis that was linked to eating contaminated blood sausage. It is from this link that we got the name botulism, which comes from the Latin word for sausage botulus. The bacterium responsible for botulism, Clostridium botulinum, was first discovered in 1895 by the microbiologist Emile Pierre van Ermengem after an outbreak linked to inadequately cured ham. The toxin was first isolated in 1928 and the toxin's ability to block neuromuscular transmission was discovered in 1949.
The medicinal use of botulinum toxin type A (Botox©) was first used medically in 1980 for strabismus (crossed eyes) and blepharospasm (excess blinking). It was approved by the FDA for these purposes in 1989. It was not until 2002 that botulinum toxin type A gained FDA approval for treatment of glabellar lines (wrinkles), the use most commonly associated with the brand. Botulinum toxin type A now has FDA indication for a wide variety of cosmetic, glandular, and musculoskeletal disorders.
The Bacteria
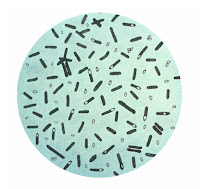 |
By Content Providers: CDC - This media comes from the Centers for Disease
Control and Prevention's Public Health Image Library (PHIL), with identification number #2107 |
Clostridium botulinum is a gram positive anaerobic bacterium that is found primarily in soil and sediment. When under stress, C. Botulinum forms spores. These spores are incredibly hardy and can survive boiling and other common sterilizing techniques. The spores remain dormant until they encounter an environment that combines anaerobic (lacking oxygen) conditions, non-acidic pH, low salt, and low sugar. Under these conditions the spores germinate and the bacterium begins to produce the botulinum toxin, which is what causes the syndrome we know as botulism.
The Toxin
A total of 7 strains of botulinum toxin have been identified. They are named toxins A-G and affect a variety of species. Toxins A, B, and E-G cause disease in humans. Toxins C and D affect mammals and birds and type E causes botulism in fish. Botulinum toxin is one of the most potent toxins known, with a median lethal dose of 1ng/kg. To put that in perspective, 1 gram of purified botulinum toxin has the potential to kill 1 million people if left untreated. It for this reason that botulinum toxin is classified as a Bioterrorism Category A (highest potency and potential risk) substance alongside anthrax, plague, smallpox, tularemia, and viral hemorrhagic fevers (such as Ebola).
Botulinum toxin works primarily at the neuromuscular junction. The neuromuscular junction is the site where nerve transmission is converted to muscle contraction. This process involves the release of the neurotransmitter acetylcholine into the space between the nerve and muscle cell. Acetylcholine is stored at the end of the nerve in vesicles. These vesicles must fuse with the cell wall in order the release acetylcholine. This fusion is dependent on a complex of proteins called SNAP and SNARE proteins. Botulism toxin cleaves these proteins and prevents fusion of the vesicle and thus acetylcholine release. The exact site on each protein depends on the strain of toxin but the end result is the same for all forms of botulism: loss of the ability to use acetylcholine to cause muscle contraction. The sites that depend on this include all voluntary muscles including the facial muscles that allow you to smile, the muscles that coordinate swallowing, the muscles in your arms and legs, and those responsible for breathing.
 |
Botulism toxin mechanism
Source: Goldfrank's Toxicologic
Emergencies 9th edition
|
Botulism Syndromes
There are 6 commonly recognized botulism syndromes that vary based on the source of toxin exposure (pre-formed toxin vs bacterial infection/colonization). These syndromes are: wound botulism, infant botulism, food-borne botulism, adult intestinal toxemia botulism, iatrogenic botulism, and inhalational botulism.
Wound botulism (15% of cases)
Wound botulism is caused by an infection of C. botulinum in the skin. It is classically associated with subcutaneous injection ("skin popping") of black tar heroin. Injection under the skin can lead to infection and abscess formation which provides the ideal environment for spore germination and toxin production. This form of botulism is most common in long term heroin users, particularly on the west coast where black tar heroin is more common.
Infant botulism (63% of cases)
Infant botulism occurs when infants <1 year old ingest C. Botulinum resulting in gut colonization due to the lack of normal gut bacteria that would prevent C. botulinum from becoming established. The bacteria in the gut then produces botulinum toxin which is absorbed in the GI tract. Infant botulism is classically associated with ingestion of honey, although this link is only present in ~20% of cases. Infant botulism is the most common form of botulism and results in ~100 cases a year in the United States.
Food-borne botulism (18% of cases)
Food-borne botulism, the form linked to the cases in Northern California, is caused by the ingestion of pre-formed toxin. This is most commonly associated with home canned foods (particularly vegetables with low acid content such as peppers, beans, mushrooms, and beats) or low acid foods that are allowed to ferment at room temperature. Approximately 39% of food-borne botulism cases in the US occur in Alaska where traditional foods such as fermented fish and fish eggs are common. Soft cheeses are also susceptible if they are improperly refrigerated, which is the suspected cause of the Northern California cases.
Adult intestinal toxemia botulism (rare)
Adult intestinal toxemia botulism is a rare form a botulism that occurs in adults and results from intestinal colonization by C. Botulinum. This occurs in persons with abnormal gut anatomy or function, or in those on antibiotics that interfere with normal gut bacteria.
Iatrogenic botulism (rare)
Iatrogenic (caused by medical exam or treatment) botulism occurs when commercially available botulinum toxin products are improperly injected. If the toxin is injected in excessive doses or in improper locations, systemic absorption of toxin may occur. This type of error most commonly occurs when injections are performed by untrained or unlicensed practitioners.
Inhalational botulism (rare)
Inhalational botulism occurs when spores are inhaled from the environment. This was previously reported in 1962 in 3 veterinary workers who inhaled toxin from animals they were caring for. Given the rarity of this type of exposure, inhalational botulism cases would be presumed to be due to bioterrorism unless a definite alternate source could be identified.
Patient Symptoms
The symptoms of botulism can be very difficulty to initially identify. GI symptoms can be confused with other forms of food poisoning and neurologic symptoms can initially be vague. This combined with the rarity of the disease makes early diagnosis of botulism difficult.
Initial symptoms
A preceding syndrome of nausea, vomiting, and abdominal pain may occur with food-borne botulism and is virtually indistinguishable from other forms of food poisoning. Wound botulism patients may have a preceding fever and may notice skin signs of cellulitis (skin infection) or abscess formation.
Incubation period
The incubation time period for progression to neurologic symptoms varies by syndrome. Food-borne, inhalation, and iatrogenic botulism have a typical incubation period of 12 hours to 10 days with most cases developing symptoms within 24-36 hours. Wound botulism has a longer incubation period of 1-2 weeks but may be longer. Infantile botulism typically occurs 3-30 days after exposure. Adult intestinal toxemia botulism is a relapsing syndrome which makes the precise incubation period difficult to identify.
Neurologic Symptoms
Botulism is characterized by a descending muscle weakness. This weakness begins in the face with the muscles around the eyes which can result in double vision. Pupils may become dilated resulting in blurred vision. Often the first symptoms that a patient will present with are facial weakness or difficulty swallowing. This weakness progresses to a descending flaccid (floppy, no tone) paralysis of the upper and then lower extremities. The most feared and life threatening complication is paralysis of the diaphragm and intercostal (between the ribs) muscles which can result in respiratory failure (inability to breath). Without treatment or supportive care, botulism carries a mortality rate of ~50%.
Diagnosis
Initial diagnosis of botulism is based on clinical symptoms and history. A combination of nerve conduction and motor testing may be helpful in differentiating from alternate causes of weakness. However these tests cannot distinguish between botulism and other causes of weakness that target the neuromuscular junction (ie myasthenia gravis, Lambert-Eaton syndrome, or the intermediate syndrome of organophosphate pesticide poisoning). Laboratory testing can be done to identify C. botulinum in the stool or botulinum toxin in the blood, stool, or food.
The standard test performed to confirm botulism is the mouse lethality assay. In this study, a sample (either serum, stool, or food sample) is injected into the abdomen of a mouse. A sample along with antitoxin is injected into a control mouse and they are observed for symptom development. This test can detect very small amounts of toxin but may take several days to complete which limits the test's utility for early diagnosis. The mouse lethality assay is more commonly used as a confirmatory test, particularly in patients receiving antitoxin therapy. Samples must be sent prior to the administration of antitoxin.
Treatment
Supportive care is the mainstay of treatment for botulism cases. Death most commonly occurs due to weakness of the muscles responsible for breathing. The strength of these muscles can be evaluated by measuring the negative inspiratory force (NIF) that a patient can produce. This test essentially measures the amount of suction a patient produces when they breath in. A force of less than -30 cm H20 represents severe respiratory muscle weakness. In such cases, a breathing tube and ventilator are often required.
In cases of wound botulism, wound debridement should be performed as soon as possible. Antibiotic therapy with penicillin will kill C. botulinum bacterial but will not prevent absorption of pre-formed toxin. Antibiotics such as clindamycin and aminoglycosides (such as streptomycin, gentamycin, neomycin, and amikacin) should be avoided as they can interfere with neuromuscular transmission.
Antitoxin
Early administration of antitoxin is critical for stopping the progression of botulism symptoms. The antitoxin binds botulinum toxin in the blood and prevents it from interfering further with the neuromuscular junction. Early treatment with antitoxin is associated with shorter duration of symptoms and decreased ventilator need. A specific form of antitoxin derived form the plasma of immunized humans is available for treatment of infant botulism. It is important to note that antitoxin only halts the progression of symptoms and will not reverse any weakness that is already present. Antitoxin is obtained from the CDC through the local health department.
Prognosis
Botulism has a highly variable duration of symptoms, in many cases lasting more than a year. Following recovery, patients with often report ongoing fatigue, dry mouth, muscles weakness, and decreased exercise tolerance. Despite these symptoms full recovery is possible with proper medical care.
DISCLAIMER
The information in this blog is for information purposes only and is not intended for use in diagnosing a disease or to provide specific treatment recommendations. For information on management of poisoned patients or if you are concerned that you have been poisoned, please contact your local poison center at 1-800-222-1222.
This Week in Toxicology is the product of James Chenoweth MD
and Daniel Colby MD. We are both board
certified in Emergency Medicine and Medical Toxicology and work at UC Davis
Medical Center as well as the Sacramento Division of the California Poison
Control Center.
References
[1] Nelson L, Goldfrank LR. Goldfrank's
toxicologic emergencies. 9th ed. New York: McGraw-Hill Medical; 2011.
[2]
Zhang JC, Sun L, Nie QH. Botulism, where are we now? Clin Toxicol (Phila).
2010;48:867-79.[3] Sobel J. Botulism. Clin Infect Dis. 2005;41:1167-73.
[4] Wikipedia. Botulism. Available at: https://en.wikipedia.org/wiki/Botulism. Accessed 5/25/2017.



Comments
Post a Comment